With the Lancet COVID-19 Commission Report published in September 2022, the global health community had a chance to pause, reflect and unlearn from experiences within the first two years of the COVID-19 pandemic. The findings and recommendations collated by 28 world-leading experts and over 100 contributors cited several ‘hard truths and ‘widespread failures’ of the global pandemic response. Indeed, astute policy recommendations coupled with the report’s concluding emphasis on “Collective action that promotes public health and sustainable development” is resounding…albeit with one very glaring omission.
The commission report does not underscore the importance of viewing health systems and the global pandemic response as Complex Adaptive Systems (CAS). In fact, the term ‘complexity’ or CAS is not mentioned in the report in any context whatsoever. In section 1, the commission provides five pillars for fighting emerging infections, including prevention, containment, health services, equity, and global innovation and diffusion. I cannot help but concur with Vivian S Rambihar’s recent assessment in the BMJ for the need for a sixth pillar: “Complexity thinking and complex systems approach to comprehend and manage pandemics and prevent the massive global errors“.
What are Complex Adaptive Systems and what is their utility as conceptual frameworks to understand pandemics?
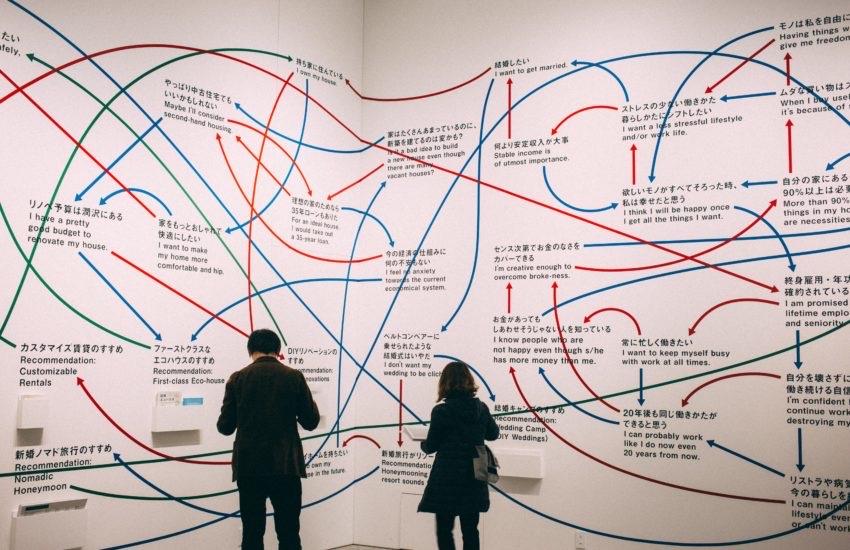
Put simply, complexity thinking and CAS framing conceptualizes emergent phenomena and societies as a set of connected interdependencies across individuals, communities and systems. Over the past two years, the pandemic has orchestrated dire provocations for our existing ways of conceptualising and responding to global threats. We have realised that the dominance of narrow framings incognisant of the social embeddedness of situations significantly circumscribes the scope of knowing and responding to so called ‘wicked’ problems.
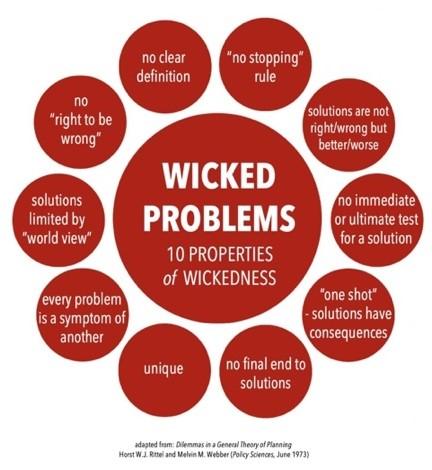
In 1973, design theorists Horst Rittel and Melvin Webber introduced the term “wicked problems” (fig 1) to draw attention to the complexities and challenges of addressing planning and social policy problems. Wicked problems have unique characteristics and lack clarity in both their aims and solutions. COVID-19 is, unmistakably, a ‘wicked problem’, the ramifications of which will be felt across generations. Developing appropriate knowledge-action configurations to abet these requires an epistemological shift towards more comprehensive and critical approaches to learning, adapting and devising appropriate resolutions. Without the gift of hindsight, planning and addressing immediate and anticipating future needs is not an easy task. Even more so in the context of crises, where the ‘what is’ and ‘what ought to be’ is so inextricably dependent on our incomplete (and ever evolving) knowledge and global political contestation.
Ever since the 2009 flagship report of the WHO Alliance for Health Policy and Systems Research, there has been a long-standing chorus for the inclusion of complexity science and systems frameworks in Health Policy and Systems Research. However, in the context of COVID-19, framing the need for complex systems approaches as a pillar for the fight against emerging infectious diseases is more urgent than ever. No pandemic has ever made so many people feel so personally, and so concomitantly connected, as we do now.
“For every complex problem, there is an answer that is clear, simple and wrong’ – H.L. Mencken
A method to the madness and the transcendent case for complex systems framing
The case for complexity goes well beyond the pandemic. Applications of methodologies like Systems Dynamics Modelling, Network Analysis, and Causal Loop Diagramming have demonstrated strong promise and policy implications in the context of advancing Universal Health Coverage (UHC), health workforce planning, emergency care delivery, primary healthcare strengthening, and multilateral agenda setting. All of which are important considerations for COVID-19 recovery, as laid out by the COVID-19 Commission report.
Even within some of the Commission’s own recommendations, e.g. – ‘The need for curative health systems to address the oft-overlooked prevalence of Non-Communicable Diseases’ – Complex systems approaches are particularly relevant but regrettably omitted as a framing lens.
While later portions of the report arguably signal complexity through the lexicon of ‘integrated’, ‘unifying’ approaches to human and animal health through a ‘One Health’ approach, its emphasis is at best implicit and limited to the context of regulations for precluding ‘spillover events’ and understanding disease origins.
In the context of COVID-19, the absence of an explicit characterization of complexity thinking as a basis to reflect on the past two years of the pandemic is a missed opportunity for vital recommendations and strengthening multilateral responses to global emergencies across UN member states, agencies, institutions, as well as in the G20 and the G7. The findings of the Commission report have revealed our collective shortcomings in pandemic prevention and response and provided us with crucial recommendations to help us navigate the path to pandemic recovery. However, we should also recognize that COVID-19 is but a microcosmic reflection of a chronic global sustainability crisis that is driven by environmental degradation, unsustainable consumption patterns, war, and anthropogenic climate change.
To understand and prevent the interconnected consequences of the pandemic, a complex, ‘Systems Thinking’ approach is required. In other words, this framing can no longer be considered as an optional ‘nice to have,’ rather, it must be actively advocated for as an overarching centrepiece for understanding the interrelated dynamics of how societies can organize themselves to mutually achieve collective health goals.