
During the closing plenary of the 2nd International Symposium on Community Health Workers (CHW) held in Dhaka, Bangladesh, from 22 to 24 November 2019, the following statement was made: “CHWs, Community Based Organisations (CBOs), leaders and other community actors, including families, can be an effective resource in fragile settings.” This solemn declaration was at least partially based on the panel discussion led by the “Community Health” Community of Practice (CH-CoP) on the first day of the Symposium. The panel, comprising some members of the platform zoomed in on community health in fragile settings (due to multiple geographical, political and economic factors), drawing on examples from Burkina Faso, Cameroon, Guinea and India.
The relevance of community health (or perhaps more accurately of communities in fragile settings) draws upon the conceptual framework of ‘negentropy’ by Edgar Morin. Morin defines negentropy (‘reverse entropy’) as the tendency of human systems towards permanent reorganisation, reconstruction or resilience, and this especially when facing trouble, disorder or crises. Fragile settings certainly seem to fit the bill.
Along these lines, the moderator of the session, Sanghita Bhattacharyya, explained the focus of the panel, highlighting the resilience of community actors when facing fragility, and this across different contexts in the world. The following points were made during the presentations and a very stimulating Q & A with the audience.
The path dependency of community health and fragility was emphasized. The “three ages of community health”, the Alma Ata Age, the Bamako Initiative Age and the New PHC Age, all show how families and communities can face different and often linked forms of fragility: colonialism, economic crisis, poverty, outbreaks, armed conflicts, climate change, … This historical perspective opens up a window of research and policy to deepen our understanding on how and in what way communities (sometimes) became more resilient in the face of very difficult situations.
Participants agreed on the important role played by CHWs in fragile settings. Evidence from the field (as well as other research) has shed more light on this assertion. We distinguish both health system related practices and community related dynamics.
Health system related practices are linked to health managers or frontline workers. Health managers and frontline workers manage the available information or knowledge on the challenging health service delivery situation in affected communities. Based on this, depending on the situation, they go for task delegation, collaboration with NGOs and/or another way of navigating the health system. For instance, CHWs are often used to provide health services in refugee camps or to Internally Displaced Persons (IDPs) in communities. Health Managers also often collaborate with NGOs as they can play a decisive health service delivery role in many fragile settings, drawing upon CHWs as well.
Besides health system related practices, one also needs to look at community related dynamics. Studies conducted in India and Guinea show that CHWs who are supported by their communities play a steady and vital role in fragile settings. In India, female CHWs known as ASHAs, demonstrate coping strategies or resilience during and after conflicts even if they themselves face plenty of vulnerabilities and challenges. For instance, they will continue doing their work when facing the loss of a family member, social rejection or strong opposition when transporting pregnant women. Sometimes, however, like in Guinea, CHWs can also face distrust from the community, as they’re seen as too close to the health system (in which people have a lack of trust). This can have a detrimental effect on health service delivery.
For effective community health intervention in fragile settings, one has to look beyond CHWs (only)
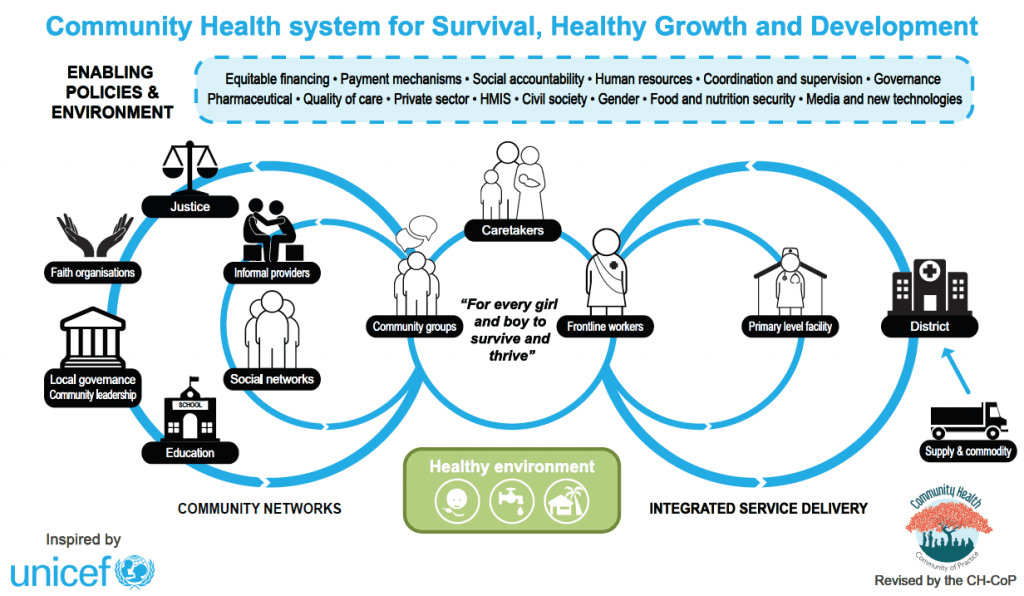
CH-CoP has always defended the idea it’s crucial to look beyond (just) CHWs for community health, especially in fragile settings. More precisely, promoting the smooth interaction of CHWs with other community structures or actors like local leaders, CBOs or local governance structures will bring more efficiency when the aim is to boost community health in fragile settings. The framework below, developed by the 450+ experts of CH-CoP, shows how, ideally, close linkage between the CHWs and various community actors ensures that they can act as a unit and facilitate service delivery.
The case of the response to the Ebola outbreak in Guinea illustrated in a study from 2016 shows that interventions like social mobilization or community engagement activities were indeed able to bridge the gap created by distrust between communities and health systems (including CHWs).
With a view on evidence based policy, more mapping studies need to be conducted to deepen the understanding of practices, dynamics and mechanisms related to CHWs in health systems and communities. By recognising the broader perspective of community health involving CHWs but also other local actors in fragile settings, the Dhaka Symposium, in alignment with the Alma Ata Declaration and more recently the Astana Declaration sounded like a forceful plea for more investment in global health and at country level, including – very much so – fragile settings. We happen to agree.

Good Job. Congrats