Tuberculosis (TB) remains the world’s leading cause of death from a single infectious agent. Combating this global epidemic requires combined actions against its five main health-related risk factors, namely, diabetes mellitus, HIV, smoking, undernutrition, and disorders due to alcohol use.
I am particularly interested in the association of TB and type 2 diabetes (T2D), the scientific evidence for which dates back to 2011, when the WHO and the International Union Against Tuberculosis and Lung Disease launched the Framework that recommends integrated services for joint management of TB and T2D.
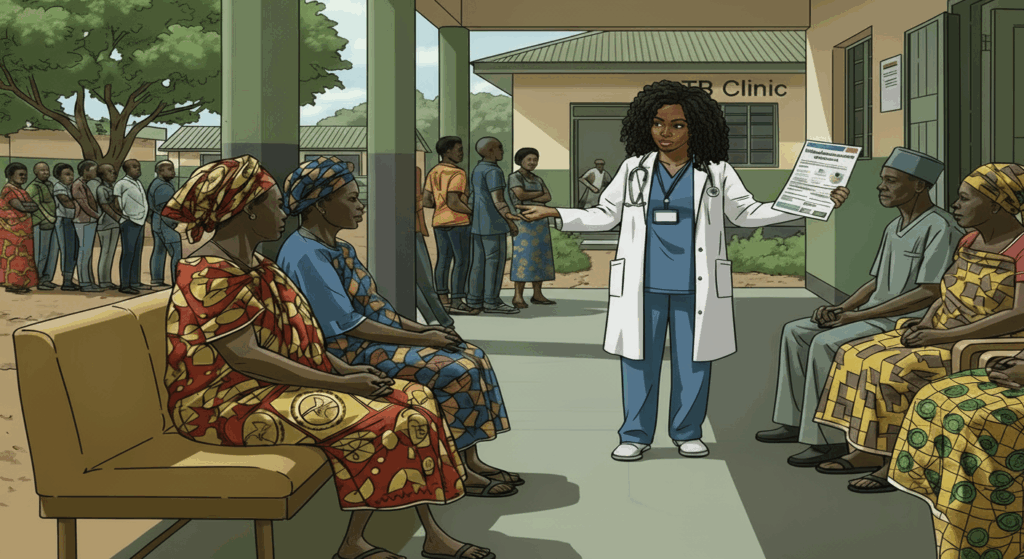
Although this Framework was already launched fourteen years ago, to date, in Mozambique, the integration of TB and T2D health services hasn’t really materialized in a more or less structured way. Integration would ideally include collaboration between TB and non-communicable (NCDs) programmes on screening, diagnosis, treatment and management of T2D in people with TB and vice-versa.
The lack of integrated action to respond to this TB-T2D comorbidity is worrying because the incidence of TB in Mozambique is estimated to be one of the highest worldwide at 361 new TB cases per 100.000 inhabitants. Additionally, data from the NCDs national survey (InCrónica 2024) indicate that from 2005 to 2024 there was an increase in the prevalence of hyperglycemia/diabetes from 3,8% to 4,1%.
Against this backdrop, I have just started my PhD in which I intend to explore as the main research question, “how can the Mozambican health system better assess and address the challenges of responding to the health care needs of individuals living with TB and T2D comorbidity?” To answer these questions, I have designed a mixed methods study that uses quantitative and qualitative methods, including a cross-sectional component, policy document review, key informant interviews, interviews with individuals who have both conditions and stakeholders’ engagement.
Lack of Integration of TB and T2D health services so far in Mozambique
The health system in Mozambique is characterized by investments by various global initiatives, mostly targeting specific infectious diseases, such as the Global Fund to fight AIDS, TB, and Malaria, or focusing on particular technologies, such as GAVI, the Vaccine Alliance. By and large – with the exception of the Global Financing Facility perhaps -, these initiatives have supported large vertical, and often fragmented programmes supporting donor goals but often without alignment of activities for enhancing effectiveness and resource allocation. Amidst all the financial challenges faced by the country (with this year not exactly ‘helping’), the donors’ prioritization of vertical programmes (till now) is, arguably, a key barrier to the effective introduction of care for emerging NCDs such as T2D, in a context of continued infectious diseases burden (the case of TB). Tuberculosis services have been mostly delivered vertically so far, with the exception of joint management of TB and HIV/AIDS.
My own experience implementing TB studies underlined the lack of perspective on early prevention, diagnosis, treatment or management of T2D in these patients. There are no guidelines for T2D screening, diagnosis and management within TB care, and even in the rare cases when screening and diagnosis is performed at the clinician’s discretion, individuals are referred to secondary or tertiary health care for follow-up, leading to delays in initiating the treatment and patients’ loss of follow-up in primary care.
In recent years, countries bordering Mozambique such as Malawi, Eswatini, Zimbabwe, Tanzania, Zambia and South Africa have been implementing studies to identify practices for integrated TB-T2D health services. Most of these integrated programmes are carried out at primary healthcare (PHC) centers, using TB clinics and/ or NCDs clinics as entry points. These initiatives make it timely to also implement research on TB-T2D integration in Mozambique, in a global context in which it has been proven that siloed responses cannot address the challenges posed by NCDs.
Changed health financing paradigm
It is true that this need for TB-T2D integration faces financial challenges, especially in an atypical year, characterized by the shock of major US funding cuts with respect to USAID (United States Agency for International Development) and PEPFAR (U.S. President’s Emergency Plan for AIDS Relief). Due to these cuts, at least 2.500 jobs were lost in Mozambique resulting in a drastic reduction of basic health services leading to numerous deaths.
In response to this changed “health paradigm”, whereby external financing of health is probably bound to remain limited, in August 2025 the government of Mozambique adopted policy measures aimed at ensuring the sustainability of essential services and stimulating the national economy. This included the redirection of public spending prioritizing allocation of resources to key sectors such as health, the mobilisation of domestic resources, support for national production, strengthening of social protection and improvement of budget management efficiency.
Even with this commitment, the reality is quite a different story, however, as Mozambique is part of the group of countries that have not been able to allocate 15% of national budgets to the health sector, according to the Abuja Declaration of 2001. From 2018 to 2022, on average health sector expenditure in relation to total expenditure was 8.4%. It remains to be seen whether this will change after the massive external health financing shock from this year.
As some scholars suggest, against the backdrop of a very difficult health financing environment, I believe it is sustainable and beneficial for people from LMICs to integrate health service delivery at the PHC level, which comprises essential health services that should be universally accessible to all.
Despite examples of successful use of integrated health services, such as TB-HIV services integration in SSA countries, tensions, and gaps across this body of work continue to exist. Tensions between the idea of unity and the diverse practices of integrated care; and gaps between expectations for what integrated care should achieve and evidence of actual change. Nevertheless, integrated care is the future, also in Mozambique. And hopefully, donors will also align with this in the coming years, as part of the Lusaka agenda .
Final thoughts
In my research idea of integrating TB and T2D, I hypothesize that integration can be implemented from TB clinics, as entry points, and established in all high-TB burden countries, including Mozambique, within the PHC level. Additionally, I will draw on lessons learned from collaborative TB and HIV/AIDS programming over the past decades.
While in this article I advocate for the integration of TB and T2D, I recognize that TB is influenced by other equally important risk factors, leading to multimorbidity among individuals with TB – a relatively new concept. But it is my sincere hope that in the future people will not be divided into fragments and will have the opportunity to receive the healthcare that meets their needs.